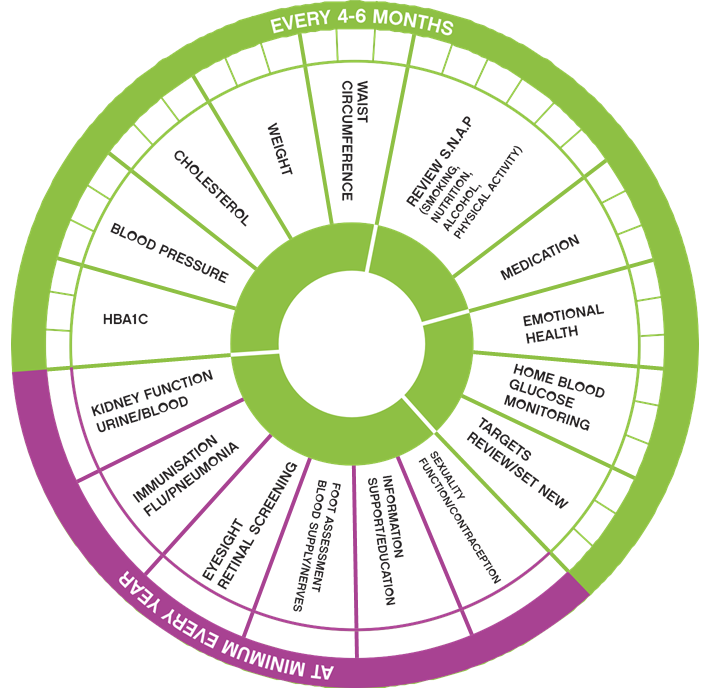
The diabetes annual cycle of care is a checklist for reviewing your diabetes management and general health. This is something that all people living with Type 2 diabetes should be aware of and know the importance of. As well as self-managing your diabetes, daily routine checkups with your GP or diabetes team are an essential part of diabetes management as it reduces your risk of diabetes-related complications.
It’s important to attend for your medical check-ups to identify any health concerns early and discuss the best treatment with your doctor or diabetes health professionals. Without regular checks, diabetes can lead to complications that can affect your whole body, including your kidneys, eyes, feet, nerves, and heart.
The annual cycle of care includes the following health checks:
HbA1c (minimum every 6 months)
This blood test reflects your average blood glucose level over the previous 10 -12 weeks.
This should be done at least every 6 months, or more often if required. The general recommendation is to aim for a reading of 53mmol/mol or less. HbA1c targets can be different for everyone so it’s important to discuss your individual HbA1c target with your doctor or diabetes nurse/practice nurse.
This test can also be carried out in selected CarePlus Pharmacies.
Blood pressure (6 months*)
Your GP or practice nurse should be checking your blood pressure at every visit or at least every 6 months, but more frequent checks can be done with your pharmacy. As a general guide, the target for people with diabetes is 140/80mmHg or less. If you have existing cardiovascular or kidney disease, your doctor will advise you on a blood pressure target to meet your individual health needs.
Research has shown that keeping blood pressure on target decreases the risk of stroke, heart, kidney and eye disease, and nerve damage.
More frequent monitoring of your blood pressure can be done in any of the CarePlus Pharmacies.
Foot assessment
Your GP, practice nurse or podiatrist should conduct a foot assessment to check the blood supply and sensation in both of your feet. If your feet have been assessed as low risk, you should have a foot assessment every year. If your feet have been assessed as intermediate or high risk, you should have a foot assessment at least every 3-6 months. Daily foot care is essential. Get to know your feet and check them every day. If you can’t reach your feet, you can use a mirror or have someone look at them for you.
For more information about how to look after your feet, talk to your GP, podiatrist or diabetes health professional or visit HSE Living with Diabetes and Footcare
Eye screening (annually or every 2 years if low risk)
Damage to the small vessels in the back of your eyes can occur even without your knowledge. That’s why it’s essential to have your eyes checked regularly by attending the National Screening Service Diabetic Retina screen.
If you do notice any changes in your vision, it’s important to contact your GP or eye specialist as soon as possible.
The National Screening Service Diabetic Retina screen offers annual free retinopathy screening. It’s for all people living with diabetes aged 12 years and older. If you have a result of no retinopathy in your previous 2 screenings, your next screening invitation will be 2 years from the time of your last screen.
If diabetic eye disease is found early, treatment can reduce or prevent damage to your sight. The longer you have had diabetes, the more likely you are to develop diabetic retinopathy.
A healthcare professional can refer you to eye screening, you can self-register at the link below, but the referral form will need to be printed and signed by your GP.
Register for your retinal screening appointment at the link here or freephone 1800 45 45 55
Kidney health (12 months)
If your blood pressure and blood glucose levels remain high over time, this can increase the risk of damage to your kidneys. Every 12 months your GP or diabetes team will arrange a urine test to check for protein in your urine (albuminuria).
A blood test to assess your kidney function is also recommended.
Cholesterol and triglycerides (12 months)
Healthy cholesterol and triglyceride levels will reduce your risk of diabetes-related complications. Your doctor will check your blood fats every 12 months
As a guide, aim for:
- Total cholesterol of less than 5mmol/l
- LDL (bad) cholesterol of less than or equal to 5mmol/l
- HDL (good) cholesterol of 1mmol/l for a man, >1.3 for a woman or higher
- Triglycerides of less than 7mmol/l.
Weight, waist, and body mass index (6 months)
If you are carrying extra weight, losing even a small amount of weight (5-10%) will help reduce your blood pressure, blood glucose levels and cholesterol.
One way to assess your weight is by using the Body Mass Index (BMI). This measures whether or not you are in a healthy weight for your height. It’s calculated by dividing your weight in kilograms (kg) by your height in meters squared (m²). You can also use online calculators to know your BMI. A BMI between 18.5 and 24.9 is within the healthy weight range.
Your waist measurement is also an important indicator of your health risks. The recommended waist measurement is less than 94cm/37 inches for men and less than 80cm/32 inches for women.
These targets are for people from European backgrounds. Different target ranges may be used if you are from different ethnic backgrounds. Speak to your doctor or diabetes health professional about the BMI and waist targets that are right for you.
Healthy eating (3-6 months)
Following a healthy balanced diet will help you achieve the best possible blood glucose and cholesterol levels, and help you manage your weight. See www.diabetes.ie for lots of helpful information on healthy eating for diabetes.
Physical activity (3-6 months)
Be physically active. For good health, aim to do at least 30 minutes of moderate physical activity (such as brisk walking, swimming, or cycling) on most, if not all, days of the week. You can exercise in shorter sessions of 10-15 minutes as it all adds up. You can also incorporate light exercise into your daily routine. For example, choose to climb the stairs instead of using the lift or hang washing outside instead of using the dryer. The best activity is one that you enjoy and gets you moving. It’s also important to limit the amount of time you spend sitting and being sedentary. Include exercises to help with muscle strengthening, flexibility and balance on 2-3 days per week.
Before starting any new exercise or activity program, check with your doctor to make sure it’s suitable for you. If you are on insulin or other glucose-lowering medications, you may need to take special precautions when exercising to prevent your blood glucose level from dropping too low (thereby increasing the risk of hypoglycaemia or ‘hypo’). Make sure you discuss this with your GP, or diabetes team Your level of physical activity will be reviewed as a part of your annual cycle of care as it is an essential part of diabetes management.
See the HSE website for some exercises you can do indoors
Diabetes self-management education
To help you with self-management of your diabetes it is also recommended that you do a structured education programme. These are free group education courses that provide the information and support to increase your knowledge, skills, and confidence in managing your diabetes. You will meet others living with diabetes and learn by sharing your experiences and listening to others. There are 3 courses available in Ireland for people with Type 2 diabetes and they are all facilitated by diabetes nurses or dietitians.
The following link directs you to available courses and how to register for one Diabetes support course - HSE.ie
You can also do an online module in the comfort of your own home. This module is called Diabetes smart and is available on the Diabetes Ireland website or on www.diabeteseducation.ie
Medication review (12 months)
A review of your medications helps ensure that you know how they work, when to take them, potential side effects and the combination of all your current medications is safe and that the doses are right for you. Medication reviews can be conducted in different healthcare service settings such as pharmacies*, primary (GP’s, nurses) and secondary care (hospitals, clinics).
Your diabetes health care team will review your overall diabetes management and provide advice on how to keep your diabetes on track.
Smoking (3-6 months)
If you are a smoker, quitting can help reduce your risk of diabetes-related complications and improve your overall health. Some people find it hard to quit, so if you feel you cannot give up smoking on your own, ask for help – talk to your GP or Pharmacist.
Other supports:
- HSE website on wellbeing and quit smoking
- Freephone tel:1800201203
- Free text QUIT to 50100
Emotional health (12 months)
Your emotional health is also important. If living with diabetes is making you feel anxious or distressed, discuss how you’re feeling with your family, friends, and diabetes health professionals. They can help you access the support you need.
You can also contact Diabetes Ireland who provide a fee-paying one-to-one counseling service. For further information, please contact 01 8428118.
Upgrade Blood Glucose Meter (24 months)
Monitoring blood glucose helps to determine if you are meeting your glucose targets which helps to reduce the unpleasant symptoms of high and low blood glucose levels and avoid long-term diabetes complications. It is helpful to remember that the numbers are neither good nor bad. They are simply information used to help you learn what is working well and identify areas for improvement in your diabetes management.
Depending on what type of diabetes you have and what treatment you’re on will determine the frequency of checking your blood glucose levels. See the CarePlus Blood Glucose Monitoring fact sheet for a test guide.
Meters may differ in use, but it is important to upgrade your meter every two years. Call into your local CarePlus Pharmacy to get your FREE OneTouch blood glucose meter today.
Vaccinations (Annually or as required)
It is extremely important for everyone with diabetes to avail of the national immunization program. Diabetes is classed as an “at-risk group” therefore all vaccinations are free to avail of for people living with diabetes under this program. All program vaccinations are available through your GP and selected CarePlus Pharmacies.
- Flu vaccine – This vaccine is free of charge as part of the National Immunisation Program for anyone 65 years old and over and anyone identified in an at-risk group, including people living with diabetes. They are available through your local CarePlus Pharmacy*, GP during the flu season which runs from October to April each year.
- Pneumococcal vaccine - The vaccine is free of charge as part of the National Immunisation Program for anyone 65 years old and over and anyone identified in an at-risk group, including people living with diabetes. The vaccine is free only through GPs. Pharmacies can offer it privately. (*Available Selected CarePlus Pharmacies only)
Note: The targets listed are for adults living with Type 2 diabetes. This information is intended as a guide only. It should not replace individual
medical advice. If you have any concerns about your health, or further questions, you should contact your health professional.
Further information on diabetes please see links below:
CALL TO ACTION: EXTEND THE TYPE 2 CYCLE OF CARE TO ALL PEOPLE
Diabetes Ireland has launched its 2022 Pre-budget submission and is proposing 8 immediate actions for implementation which will improve the quality of life for over 225,000 people living with diabetes and reduce the long-term costs of preventable diabetes complications. The submission is focused on a range of deliverable actions that are person-centered, cost-effective and build on existing HSE commitments to tackle chronic conditions including diabetes. For further information please visit Diabetes Ireland website.
Information from Diabetes Ireland


